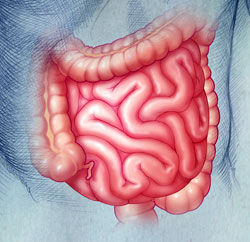
Celiac disease, also known as Celiac sprue, is a medical term that describes a condition found in individuals with an inappropriate immune response to gluten, a protein found in wheat, barley, and rye. The reaction causes inflammation in the lining of the small intestine, which is the part of the body between the stomach and large intestines where nutrients are absorbed. As a result, many people with celiac sprue may develop signs of malabsorption because the bowel becomes inflamed and will not properly absorb nutrients. In this case certain complications may arise including iron deficiency anemia, osteoporosis, bone fractures, defects in dental enamel, infertility, miscarriages or menstrual irregularity, impaired blood clotting and recurrent sores in the mouth.
The disorder is also known as nontropical sprue, idiopathic sprue, celiac disease, gluten-sensitive enteropathy, and gluten-induced enteropathy.
FAQs
Symptoms include but are not limited to:
- Vomiting
- Poor appetite
- Bloating
- Flatulence
- Abdominal pain
- Diarrhea
- Constipation
- Weight loss
The cause isn’t known, but the condition does have a genetic basis and frequently occurs within families. Celiac disease results from the interaction between dietary gluten and specific immune, genetic, and environmental factors.
Celiac disease can affect one in 100 individuals. It is slightly more common among people of western European ancestry. There is an increased prevalence in first-degree relatives and other various autoimmune conditions.
There are several blood tests that screen for very specific elements that indicate Celiac disease. A diagnosis is usually confirmed with a biopsy of the lining of the small intestine. The biopsy is taken during a procedure called an upper endoscopy.
Because of the nature of the symptoms of Celiac disease and because the symptoms overlap with the symptoms of other gastrointestinal disorders, it can be difficult to diagnose. Your physician may also test liver and kidney function as well as other general blood tests to rule out other conditions with similar symptoms.
Current treatment for Celic disease requires strict adherence to a gluten-free diet. This means a substantial change in diet, because in addition to wheat, barley and rye, many processed and convenience foods are made with additives and preservatives that contain gluten or related products. Beer, lagers, ales, and stouts must be avoided, although wine, liqueurs, most ciders and spirits, including whiskey and brandy, are permitted. Switching to products that contain only rice, corn, maize, buckwheat, potato, soybean, or tapioca flours is highly recommended.
Your physician and nutritionist can make additional suggestions and help guide you in making this dietary change. Only in patients that do not respond to dietary restrictions, which is rare, are anti-inflammatory medications used.
There is no cure for Celiac disease. The only way to prevent an autoimmune response is to stay on a gluten-free diet. The good news, though, is that the small intestine can heal itself and resume normal absorption of nutrients within several months of changing and closely monitoring what you eat. This is referred to a quiescent or remission state.
Your symptoms may come back.
Yes. Some adults may have a painful, itchy, gluten-sensitive skin rash called dermatitis herpetiformis that causes raised red blotches on the elbows, knees and buttocks. Insulin-dependent diabetes, liver enzyme abnormalities and thyroid disorders may also be associated with celiac sprue. If the inflammation in the small intestine is not controlled, people with the allergy also have a greater risk of non-Hodgkin’s lymphoma, osteoporosis and intestinal malignancies. These risks can be reduced by avoiding all products containing gluten.
Yes. Because Celiac disease is a life-long condition, it’s important to maintain regular check-ups to monitor your nutrition and overall health.